Written By Danielle O’Connor ND
What a confusing time, one day i feel like myself, energetic, optimistic and feeling great, and the next i’m impatient, fatigued, cranky, bloated and feeling like a hot mess. Did i do something different? I’m still eating the healthy foods and getting my exercise in, going outside for fresh air and spending time with loved ones, so why the change in how i feel? Thinking back there hasn’t been many changes, i’ve maintained my regular routine, but for some reason my body is telling me something is ‘off’.
Do you ever feel this way, not like yourself? OK, next step, off to the doctor we go to get checked out. Blood pressure checked, blood sugar good, no physical signs that they see…I’ve been checked out and yes, i’m healthy, there’s nothing wrong with me??? What?? ? How can this be, there’s something going on but everything on paper checks out. Being sent home with no answers, no direction, no insight into why you’re feeling this way can be frustrating, why can’t you get any answers.
As women, it’s time we take our hormonal health into our own hands, feeling unwell and not knowing why is not helping us out in any way, it’s time for answers, it’s time to take action and understand what’s going on in our own bodies.
Perimenopause varies greatly from one woman to the next. The average duration is three to four years, although it can last just a few months or extend as long as a decade.1
Perimenopause can be a very trying time as many women don’t feel changes in their hormones, they are still getting a regular period, they get PMS, breast tenderness, and all of the other symptoms that come along with a regular period…but their hormone levels could be decreasing slightly every day. See, throughout our hormonal life we are constantly fluctuating, but from our teens into our forties those fluctuations are consistent. What many women don’t realize is that perimenopause is like a second puberty. Remember what puberty was like, irregular periods, sometimes heavy, sometimes light, cramping, headaches, and no consistency to it at all. When you take a look at what’s happening with your perimenopausal hormones, it’s like puberty again, your hormones are all over the place, sometimes high, sometimes low, and your body is taking all the hits trying to figure out how to keep everything regulated so that big functions like breathing, digestion and immunity don’t faulter.
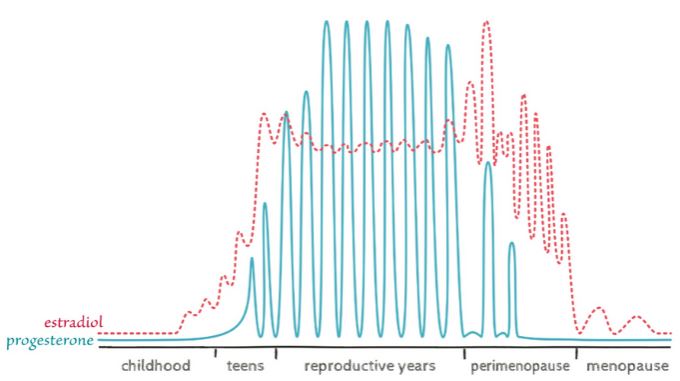
CREDIT: L. BRIDEN / HORMONE REPAIR MANUAL 2021
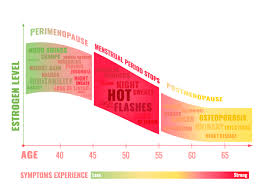
So perhaps you don’t think you’re in perimenopause, but maybe you are experiencing some very vague things like fatigue and changes to your skin. Here’s a list of symptoms that are associated with perimenopause, and it’s not just changes to your period.
Perimenopause symptoms: 2-25
| Headaches | Burning mouth | Change in taste |
| Fatigue | Bloating and other digestive issues | Joint pain |
| Muscle aches | Itchiness | Difficulty Concentrating |
| Memory lapses | Thinning Hair | Brittle Nails |
| Weight Gain | Dizzy spells | Allergies |
| Body odour | Irregular heartbeat | Anxiety |
| Irregular periods or skipping periods. | Periods that are heavier or lighter than usual. | Hot flashes |
| Vaginal dryness and discomfort during sex. | Urinary urgency (needing to urinate more frequently). | Sleep problems (insomnia). |
| Changes in mood like irritability, depression or mood swings. |
Wow, with that list of symptoms it’s surprising that every woman doesn’t feel like they’re in perimenopause! We know as our hormones start to fluctuate and ultimately decrease, especially estrogen, these changes and symptoms start to develop even more. According to the National Institute of Aging, menopause typically occurs between 44-55 years old26, with the average age of 51, and perimenopause occuring for 4-8 years prior to this27.
So, obviously as women this is something that we will all encounter, in some form or another, just like puberty. So instead of suffering through and allowing this stage in our hormonal lives to take over, we have to stand up for ourselves and take control of our own hormonal health. There are a number of tools and techniques that can help us transition through these hormonal fluctuations, that in the end will make us healthier, stronger, and allow us to feel like ourselves again.
Tips for managing perimenopause:
- Eat a diet rich in soy – Studies have demonstrated the beneficial effect of soy isoflavones on menopausal mood symptoms and fatigue28
- Regular exercise – studies show women with moderate to high levels of physical activity had less severe symptoms than those who were inactive29
- Learn Mindfulness and breathing techniques for relaxation – found to reduce stress, reduce anxiety, improve sleep quality, and reduce hot flashes30,31
- Herbal supplements to consider:
- Bio-identical Hormone Replacement Therapy
It’s time to stop suffering and take control of your hormonal health, find out what treatment options will help you feel your best again. Start feeling like ‘you’ again!
Contact Dr. Danielle ND at info@drdaniellenatruopath.com if you have questions about your own homrone health.
Get your FREE perimenopause meal plan HERE
As an Amazon Associate I earn from qualifying purchases.
References:
- Harvard Health. Perimenopause. https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
- Cleveland Clinic. Perimenopause. https://my.clevelandclinic.org/health/diseases/21608-perimenopause
- Bremer, E., et al. (2019). Anxiety in menopause: A distinctly different syndrome? [Abstract]
https://www.npjournal.org/article/S1555-4155(18)31172-3/fulltext - Bromberger, J. T., et al. (2013). Does risk for anxiety increase during the menopausal transition? Study of Women’s Health Across the Nation (SWAN).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641149/ - Burger, H., et al. (2007). Nomenclature and endocrinology of menopause and perimenopause [Abstract].
https://www.tandfonline.com/doi/abs/10.1586/14737175.7.11s.S35 - Chessa, M. A., et al. (2020). Pathogenesis, clinical signs and treatment recommendations in brittle nails: A review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994568/ - Chopra, S., et al. (2019). Weight management module for perimenopausal women: A practical guide for gynecologists.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6947726/ - Dahiya, P., et al. (2013). Burning mouth syndrome and menopause.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3570906/ - Fait, T. (2019). Menopause hormone therapy: Latest developments and clinical practice.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6317580/ - Freedman, R. R., et al. (2014). Menopausal hot flashes: Mechanisms, endocrinology, treatment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612529/ - Gava, G., et al. (2019). Cognition, mood and sleep in menopausal transition: The role of menopause hormone therapy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6843314/ - Goluch-Koniuszy, Z. S. (2016). Nutrition of women with hair loss problem during the period of menopause.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4828511/ - Hot flashes: What can I do? (2017).
https://www.nia.nih.gov/health/hot-flashes-what-can-i-do - Ji, M.-X., et al. (2015). Primary osteoporosis in postmenopausal women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5643776/ - Kołodyńska, G., et al. (2019). Urinary incontinence in postmenopausal women – Causes, symptoms, treatment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6528037/ - Naumova, I., et al. (2018). Current treatment options for postmenopausal vaginal atrophy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6074805/ - Pavlović, J. M. (2018). Evaluation and management of migraine in midlife women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527322/ - Roman-Blas, J. A., et al. (2009). Osteoarthritis associated with estrogen deficiency.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2787275/ - Shah, S. (2012). Hormonal link to autoimmune allergies.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3658477/ - Suri, V., et al. (2014). Menopause and oral health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4195183/ - Taylor-Swanson, L., et al. (2018). The dynamics of stress and fatigue across menopause: Attractors, coupling and resilience.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5866170/ - Thornton, K., et al. (2015). Menopause and sexuality.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5994393/ - Vieira, A. T., et al. (2017). Influence of oral and gut microbiota in the health of menopausal women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5625026/ - What causes hot flashes? (2021).
https://www.breastcancer.org/tips/menopausal/treat/hot-flashes/causes - What is menopause? (2017).
https://www.nia.nih.gov/health/what-menopause - National Institute of Aging. https://www.nia.nih.gov/health/what-menopause
- The North American Menopause Society. https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal#:~:text=The%20average%20age%20is%2051,after%20the%20final%20menstrual%20period.
- Ahsan M, Mallick AK. The Effect of Soy Isoflavones on the Menopause Rating Scale Scoring in Perimenopausal and Postmenopausal Women: A Pilot Study. J Clin Diagn Res. 2017;11(9):FC13-FC16. doi:10.7860/JCDR/2017/26034.10654
- Dąbrowska-Galas M, Dąbrowska J, Ptaszkowski K, Plinta R. High Physical Activity Level May Reduce Menopausal Symptoms. Medicina (Kaunas). 2019;55(8):466. Published 2019 Aug 11. doi:10.3390/medicina55080466
- Johnson A, Roberts L, Elkins G. Complementary and Alternative Medicine for Menopause. J Evid Based Integr Med. 2019;24:2515690X19829380. doi:10.1177/2515690X19829380
- National Institute of Aging. https://www.nia.nih.gov/health/hot-flashes-what-can-i-do